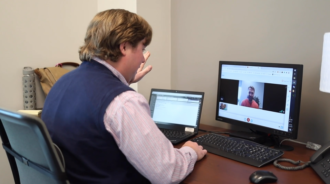
Mark Kevern of the Arden-based Compass Physical Therapy logs on to his computer as his next patient appears on screen, sitting at home. Watching carefully, Kevern coaches the person through a series of exercises.
Simply by pressing a few buttons, Kevern then pulls up a video from the secure database’s library. The patient watches as the video outlines each step in a new exercise that’s being added to the regimen.
At the start of the COVID-19 pandemic, Kevern admits he was skeptical: Could telehealth really become a viable alternative to in-person care — especially for physical therapy, a notoriously hands-on form of medicine?
The answer has been a resounding yes. Heralded as the future of medicine, telehealth was already on the rise pre-pandemic, but COVID-19 has made it the new normal. Patients are ditching crowded, potentially germ-infested waiting rooms en masse, opting to talk to their providers from the privacy and comfort of their home. Whether it involves primary care, specialty consultations, therapy or follow-up appointments, practitioners are embracing virtual care as the next best alternative to a clinical setting.
“We’ve all had to adjust and adapt,” says Kevern, reflecting on the changes of the past year. “For some people, it’s either telehealth or they don’t get any services. Through this shift, we’ve found that telehealth was actually quite effective and quite productive.”
Pandemic priorities
An estimated 7 million Americans used a telehealth service in 2019; as of April 2020, telehealth visits in the United States were on track to top 1 billion by year’s end, according to analysts at the Massachusetts-based Forrester Research. A September report by the physician network Doximity ranked North Carolina second in the United States for telehealth service expansion.
Before the pandemic, most insurance companies wouldn’t consider paying for online visits, says Shane Lunsford, administrative director of the department of psychiatry at the Asheville-based Mountain Area Health Education Center. If a telehealth visit was covered, both doctor and patient had to be at a licensed medical facility during the virtual appointment.
But as it has with so many other aspects of daily life, COVID-19 has reshaped both the industry’s attitude toward telehealth and the way it’s provided. As soon as the United States entered a federal state of emergency on March 13, 2020, major insurance companies altered their reimbursement policies to treat telehealth visits conducted from policyholders’ homes the same as in-person appointments. Strict guidelines concerning what constitutes telehealth are loosening too, says Lunsford: Phone conversations with a health care practitioner have also gained at least temporary acceptance.
According to the American Hospital Association, 35 states plus the District of Columbia have enacted laws requiring health insurers to provide the same coverage for telehealth visits and in-person services. North Carolina hasn’t done so, notes Lunsford, though in 2018, state lawmakers did open the door to enabling Medicaid patients with behavioral health and addiction issues to receive telehealth care from a licensed mental health professional.
Blue Cross and Blue Shield of North Carolina, the state’s largest private health insurer, expanded telehealth coverage last year and will continue to cover such visits the same as in-person medical appointments through June 2021, said company spokesperson Jami Sowers. In the initial months of the pandemic, the company saw telehealth claims increase by a staggering 7,000%, she said.
Hospitals hop on board
Last winter, AdventHealth Hendersonville was just starting to plan for a jump into the waters of virtual care, recalls Christy Sneller, vice president of physician services. Within two weeks of the first diagnosed COVID-19 cases in North Carolina, the hospital’s parent company launched a live telemedicine platform bringing primary, pediatric and behavioral health care into patients’ living rooms.
Now, roughly 10% of all daily visits at AdventHealth Hendersonville are conducted virtually. Many of the specialties on offer — including neurology, cardiology, endocrinology and rheumatology — have embraced telehealth for follow-up appointments.
Meanwhile, a group of critical care physicians based elsewhere in the state is on call to consult virtually with staff working in the intensive care unit, Sneller adds. Moving forward, the hospital system is looking at ways to tap into the hospital chain’s national network of specialists for virtual consultations on individual cases.
“Access is so important to patients’ receiving good quality care. If telehealth is increasing that access, I hope insurance companies will see how valuable that is,” notes Sneller. “This kind of access to preventative care is the key to keeping people from getting really serious conditions that end up costing the insurance companies a lot more money.”
The U.S. Department of Veterans Affairs has long been a leader in virtual care. In 2015, VA hospitals provided 2.1 million telemedicine consultations to more than 677,000 veterans, according to a December 2018 article in the Cleveland Clinic Journal of Medicine. Between February and May of 2020, the number of telehealth visits conducted via the national VA Video Connect platform increased by more than 1,000% per week, the federal agency reported in June.
In the Asheville area, telehealth appointments are available in almost all specialties offered at the Charles George VA Medical Center, including orthopedics, urology, neurology and an increased volume of mental health visits, says telehealth coordinator Brittany Brannigan.
“A number of our veterans have found that virtual care removed barriers in ways they didn’t expect,” she explains. “Some of our veterans have transportation issues, or they can’t take time off of work to come to their appointments. With virtual care, they can have an appointment with their provider on their lunch break, or while they’re at home taking care of their children, and they’re not having to find a ride through an organization like Mountain Mobility.”
Expanding access
The chaos and uncertainty of 2020, says Lunsford, resulted in more mental health visits and substance-use concerns than any other year on record. Because virtual appointments tend to be shorter and offer greater flexibility, more people can receive therapy and mental health support, he points out. MAHEC’s psychiatry department is now conducting 97% of its visits remotely, Lunsford estimates.
The VA has seen a similar trend, says Brannigan. The hospital’s social services department, she notes, has a program that gives iPads to veterans who can’t afford to buy a device. Some of the recipients have never used a tablet before, and the Department of Veterans Affairs offers technology consultations, both remotely and in person, to teach newbies how to use online platforms. Veterans can also bring their own devices to the local VA facility for digital literacy coaching by a staff member.
Over at Compass Physical Therapy, virtual appointments have accounted for anywhere from 5% to 25% of the office’s caseload, says Kevern. Some practices, such as dry needling and joint mobilization, can’t be done virtually, but those limitations are offset by some surprising benefits. One is the ability to see the physical layout of a patient’s home.
“We can observe them doing their exercises in their own space and talk them through their activities,” he says. “Maybe while you’re sitting in your living room you’re reminded that your shoulder hurt while putting away dishes last night, and that brings up a talking point on how to modify that activity. That link to the home environment can be really beneficial.”
Telehealth can also help when folks relocate but continue receiving care from their Asheville-based doctors, notes Lunsford. As the pandemic has dragged on, a handful of MAHEC patients have moved out of the area to be closer to family, he reports. Virtual appointments can also more readily include multiple practitioners in a single session. He cites a recent visit involving several members of a family, two psychiatrists, a psychotherapist and a family health practitioner, saying, “It becomes easier to have these conferences with a patient, and not everybody has to be in the same location.”
Still, there are trade-offs, stresses Erin Stefanacci, a chiropractor at Carolina Holistic Health. Although patients may feel more comfortable at home, she’s noticed a “different energy” when people are speaking through a computer. This, she believes, has resulted in lower quality physician/patient relationships. In addition, equipment that’s commonly found in doctors’ offices isn’t typically available in people’s homes. “If someone has a condition like high blood pressure, there is no way to see that through a video conversation,” she points out.
Unstable connection
In Western North Carolina, however, telehealth’s biggest obstacle is the lack of consistent broadband connectivity. Both Lunsford and Brannigan say unreliable cellular service in parts of the region significantly limits those residents’ access to digital services. “As soon as you leave the major highways and get out in the rural areas, coverage becomes spotty, and it’s hard for patients to connect,” says Lunsford.
In December, state legislators agreed to set aside $30 million to support broadband availability in rural North Carolina. The funding will support 18 infrastructure projects with the goal of connecting 15,965 homes and 703 businesses to high-speed internet.
Broadband aside, though, a bigger question remains: Post-pandemic, will insurance companies still see telehealth as a viable — and even essential — medical delivery system?
For disciplines such as physical therapy, the answer may depend on the success rate of virtual appointments. “Right now, we’re trying to do our best to provide value for the patient during these sessions,” says Kevern. “Hopefully, if that happens with regularity and the patient can convey feedback to the insurance companies that these services are beneficial and effective, that will likely affect coverage moving forward.”
Sneller of AdventHealth Hendersonville, however, believes the financial benefits of readily accessible preventive care may be enough to point insurance providers toward lasting policy changes: Access to quality care will ultimately save those companies a lot of money.
“If we don’t keep people healthy through their blood pressure checks, their congestive heart failure checks, through behavioral care and screening for dementia, we’re going to end up in a really big crisis down the road,” she predicts. “And virtual telehealth platforms are what has allowed us to keep all these services going.”



Before you comment
The comments section is here to provide a platform for civil dialogue on the issues we face together as a local community. Xpress is committed to offering this platform for all voices, but when the tone of the discussion gets nasty or strays off topic, we believe many people choose not to participate. Xpress editors are determined to moderate comments to ensure a constructive interchange is maintained. All comments judged not to be in keeping with the spirit of civil discourse will be removed and repeat violators will be banned. See here for our terms of service. Thank you for being part of this effort to promote respectful discussion.