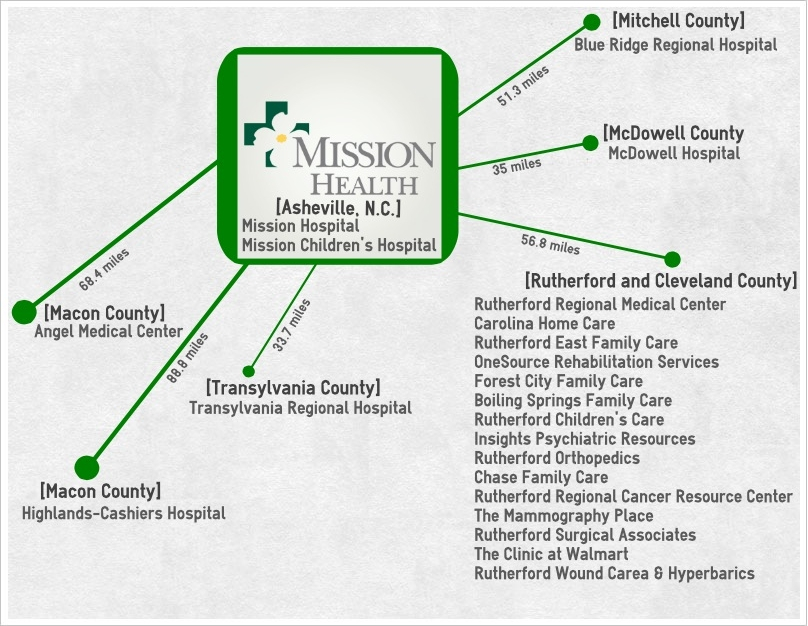
An accelerating trend: After its two most recent affiliation announcements with Highlands-Cashiers Hospital and Rutherford Regional Health System, Mission Health now boasts eight affiliates in Western North Carolina.(Graphic by Caitlin Byrd)
When a young Philadelphia physician and his wife purchased the Rutherford Military Institute property for $1,500 in 1906, Dr. Henry Norris knew he wanted to transform the former military school into a hospital that would provide quality health care to the folks who lived in the rural mountains of Western North Carolina.
Seven months later, it was so.
But as history tells us, the hospital would not remain in the remodeled military school — it would grow. For more than a century, the hospital embraced growth as it expanded in size and specialties — beginning in 1911 when it invested $100,000 in a new brick building.
The hospital eventually became Rutherford Regional Health System, which includes a network of 14 affiliates in Rutherfordton, Spindale, Forest City, Mooresboro, Caroleen and Boiling Springs, N.C.
On Sept. 20, however, the health system’s direction changed course when Mission Health announced that Rutherford Regional Health System voted to pursue a full affiliation with the Asheville non-for-profit health system, the sixth-largest health system in the state.
Eight days later, Mission Health made another announcement: Highlands-Cashiers Hospital would also seek affiliation with Mission Health.
The story of hospital mergers, affiliations and consolidations has become a common tale across the state and the country — and there’s no ending, happy or otherwise, in sight, says Don Dalton, spokesman for the North Carolina Hospital Association.
“Consolidation is not only an ongoing trend, but it is an accelerating trend,” he states.
Six years ago, 68 percent of member hospitals in the North Carolina Hospital Association were in a health system, Dalton says. Today, he reports, 85 percent of the 103 member hospitals are in a health system, which the American Hospital Association defines in two ways. A health system can be either a multihospital system like Mission Health (in which two or more hospitals are owned, leased, sponsored or contract-managed by a central organization), or a diversified single-hospital system.
And more often than not, Dalton says, rural hospitals are the institutions seeking these affiliations with larger health systems. Under the Affordable Care Act, pressures on hospitals are twofold: First, there are incentives for hospitals to integrate into accountable care organizations with physicians and other hospitals. Second, financial penalties await hospitals that have higher rates of Medicare recipients who are readmitted to the hospital after their initial discharge.
However, not all affiliations are created equal — including the ones Mission Health reached with Highlands-Cashiers Hospital and Rutherford Regional Health System.
Highlands-Cashiers Hospital’s affiliation with Mission Health is what is known as a management affiliation. In this arrangement, Mission Health provides Highlands-Cashiers Hospital with management services. However, the hospital retains ownership over its assets and maintains its employees. Only upper-level executives such as the chief executive officer and chief financial officer become part of the Mission organization.
With the full affiliation that Rutherford Regional Medical System is pursuing, Mission Health acquires the assets of the institution and essentially becomes the owner. Mission Health President/CEO Ron Paulus explains it this way: “The management relationship would be like a dating relationship, and the full affiliation is more like marriage. “At the end of the management agreement, Highlands-Cashiers could say, ‘That was fine, but we don’t really want to do it and we’re going to go back to doing our own thing.’ Whereas in the full affiliation with Rutherford Regional, the unwinding is a much more challenging thing,” Paulus says.
Dalton notes that the devil is in the details when it comes to these kinds of agreements between hospitals and health systems.
“Every situation is unique and it’s tailored to meet the needs of the two parties that are involved — the system and the hospital and whoever else may be involved,” Dalton says. “There is just no cookie-cutter approach to how very unique communities and their hospitals align themselves.”
And, these affiliations come at a price.
“It comes at a cost of their autonomy, but with the benefit of bringing to the table access to capital and access to expertise that they might not be able to afford on their own,” Dalton says.
Since McDowell Hospital became a full affiliate of the Mission Health System in 2004, Paulus estimates that Mission Health has invested more than $20 million in the health care facility — an amount he thinks McDowell may not have been able to obtain otherwise.
“The days of an individual hospital are effectively over. It’s just not enough to be a single hospital, and the smaller you are, the harder it is to be single hospital,” Paulus says. “You have to get to a certain scale in terms of credit rating and reliability and trust with a management team and those kinds of factors to get access to capital.”
Also, in many cases, having a larger system affiliation can help smaller hospitals when negotiating payment and insurance rates.
“They just don’t have the same experience base and the same ability to call on the expertise that they would need to, and they have a less of an understanding of what a fair rate is and what a fair rate isn’t. It’s easier for them to be taken advantage of, and we do our best to make sure none of our facilities in our system are taken advantage of,” says Paulus.
But, Dalton explains, health systems like Mission Health can benefit from these affiliations with rural hospitals, too.
“The larger systems also gain in terms of their reach into markets where they may not have been as strong. They also broaden the number of institutions they represent when they sit down to set payment rates with insurers, and the larger hospitals recognize that it is in their best interest and everybody’s best interest in our state to keep the smaller systems viable in our communities,” Dalton explains.
In essence, without these affiliations, rural hospitals could go out of business, leaving a community without access to a local health care institution.
Paulus says that growing Mission’s market share does not reflect the thinking behind recent or past affiliations.
“Our core goal is not about what size Mission should be, it’s about what are the needs of the residents of Western North Carolina,” Paulus says. “I don’t want to enter into multiple states or span the whole state. Our goal is to focus on Western North Carolina. Our motivation is really a community-based motivation that says our reason to exist is to serve this region, and that anything we can do within reason to help those that would like to be helped by us, we would like to do.”
Even when Mission Health was recently approached by an undisclosed larger health system, Paulus says this local focus to serve Western North Carolina residents guided his decision to decline the affiliation offer.
With the addition of Highlands-Cashiers and Rutherford Regional, Mission Health will have eight affiliations. Though Paulus says he cannot put a numerical cap on how many affiliates would be too many, he says that he follows certain guidelines when thinking about new affiliations.
“For me to grow, it would have to be in a geographically related area, either by an extension of our existing area or where there was an over-critical mass where you could already develop a regional network in some other area, and those are few and far between,” he says.
But whether these affiliations are management affiliations or full affiliations, Paulus says each one presents a risk.
“You’re taking on more responsibility. Most of the times when affiliations happen, it’s because there are challenges in the market,” he states. “We’re taking on a challenge that is something that’s hard work to do. There’s always the chance that things won’t work out.”
But it’s a chance, Paulus argues, local hospitals must be willing to take to survive in the changing health climate. “We’ve gotten to a model in our country and in Western North Carolina where it’s not really viable for any given hospital to be on its own,” he states. “The issue is not about can we go to the past, the issue is can we create our own future.”
He elaborates, “When you’re creating your own future, you want to be side by side with people you like, with people who care about the things you care about and who are in it for the long run; who aren’t in it for the money, who aren’t in it for it to get bigger, to get paid more, to gain bigger status and all that. That’s why I think Mission’s sole goal is to serve Western North Carolina. That’s all we’ve ever done, and that’s all we ever want to do.”
Send your health-and-wellness news and tips to Caitlin Byrd at cbyrd@mountainx.com or mxhealth@mountainx.com, or call 251-1333, ext. 140.



Before you comment
The comments section is here to provide a platform for civil dialogue on the issues we face together as a local community. Xpress is committed to offering this platform for all voices, but when the tone of the discussion gets nasty or strays off topic, we believe many people choose not to participate. Xpress editors are determined to moderate comments to ensure a constructive interchange is maintained. All comments judged not to be in keeping with the spirit of civil discourse will be removed and repeat violators will be banned. See here for our terms of service. Thank you for being part of this effort to promote respectful discussion.