by
Three staff neurologists are leaving Mission Hospital by the end of September, potentially leaving only two to provide critical care to hundreds of patients at the Asheville flagship hospital and across Western North Carolina, including many who have suffered strokes.
The departing physicians are neurohospitalists, specialists who treat patients in the hospital who are suffering from diseases of the brain, spinal cord and nervous system. They cover patients in general admission and the intensive care unit (ICU) and respond to strokes throughout the hospital. They also provide 13 regional hospitals with telestroke services, remotely consulting on stroke patients while teams at those sites do hands-on work.
Seven such specialists were working full time or part time at Mission as recently as the end of 2023. The decline mirrors other widespread departures from the hospital, including recent losses in its urology and medical oncology programs.
Asheville Watchdog interviewed departing physicians, who spoke on condition of anonymity because of concern for their careers or potential retribution. Their departures — triggered by what they describe as an ever-increasing patient load, Mission’s yearslong inability to hire more physicians and pay issues — intensify an exodus from the HCA Healthcare-owned hospital and a program that has been recognized nationally.
“It was just extreme burnout, plain and simple,” one of the neurologists told The Watchdog, adding that the department’s current state “feels like the end of a golden era.”
“The demands on each individual neurologist were incredible, and it was rare that we could conclude one emergency without being interrupted by another emergency,” the neurologist said. “It was with immense sadness and regret that I resigned, and I have been wrestling with the guilt of letting patients in WNC and my colleagues in the hospital down.”
Mission Hospital also plans to make significant changes to its neurology services in September, according to a complaint to the N.C. Department of Health and Human Services (NCDHHS) obtained by Asheville Watchdog and verified by the departing neurologists.
- There will be no neurohospitalists on-site overnight, and after-hours critical care will be handled remotely by a contracted telemedicine company. There will be locum tenens — temporary neurologists at the hospital — the departing physicians confirmed, but those are restricted to floor duty and not involved in critical care.
- HCA is considering making neurology solely a consult service. If it does this, it would remove admission responsibilities from neurologists, according to one of the departing physicians, who described the potential change as a positive one because it could help the hospital recruit more neurologists.
Collectively, the departing neurologists have more than three decades of experience at Mission. One worked there for three years, one for eight, and one for nearly 20.
N.C. Attorney General Josh Stein sued HCA in December 2023 for allegedly not following commitments mandated by the Asset Purchase Agreement (APA) related to its purchase of Mission Health for $1.5 billion in 2019, specifically promises to maintain emergency department and cancer care services that were in place at the time of the sale.
As modified by Stein as a condition of his assent to the deal, the APA requires that HCA maintain Mission’s general medicine services for 10 years after the purchase. General medicine, according to the agreeement, includes “hospitalist, gastroenterology, infectious disease, nephrology, pulmonary/critical care, neurology, and palliative care” services. The original agreement negotiated by the Mission board of directors required HCA to maintain the services for five years.
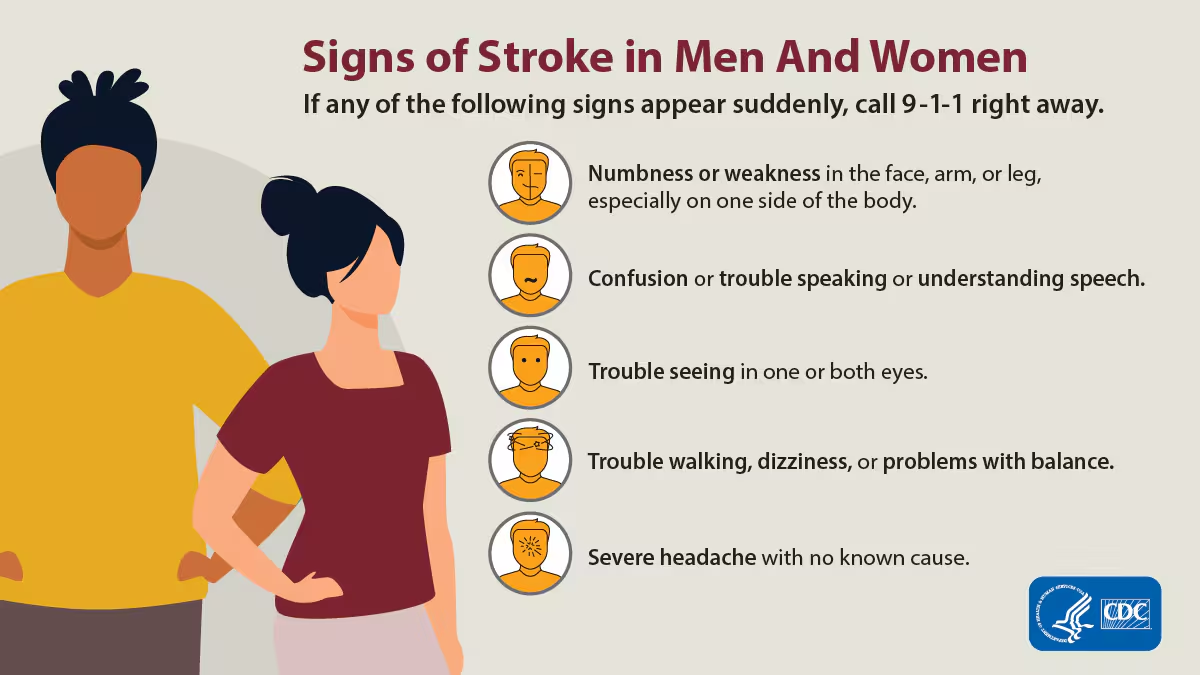
Nearest comprehensive stroke center is in Greenville
Mission’s Advanced Comprehensive Stroke Center is the only such operation serving WNC. The nearest such center outside of Asheville is at Prisma Greenville Memorial Hospital, almost 70 miles away in South Carolina. The closest in-state centers are the Carolinas Medical Center and Novant Health Presbyterian Medical Center, both in Charlotte and about two hours away.
Mission’s stroke program has also been recognized for more than a decade as an award-winning service at the hospital.
The Watchdog asked Mission Health spokesperson Nancy Lindell more than a dozen questions about the impending departures, including what the hospital system did to try to prevent them and if it would fill empty positions with permanent hires or rely on locum tenens. The Watchdog also asked her about the hospital’s plans to make changes to its neurology services.
Lindell did not respond directly to most of the questions, instead giving a blanket statement about the hospital’s neurology services and maintaining there would be no decline in care.
“Mission Hospital has 24/7 coverage which includes on-site neurologists, hospitalists, an emergency care team, critical care team, interventional radiologists, neurosurgeons, and telehealth physicians,” Lindell said. “We continue to actively recruit new physicians, and our neurology treatment will remain seamless throughout these program changes.”
The Watchdog also asked Lindell if the dwindling staff could threaten Mission’s Advanced Comprehensive Stroke Center status, accredited through The Joint Commission, an independent, not-for-profit national organization that sets standards for safety in health care.
“Mission Hospital is and remains a comprehensive stroke center,” Lindell said.
The Watchdog also asked NCDHHS whether it was investigating the complaint it had received. A spokesperson said the department could not comment because complaints are confidential.
“We cannot provide comment on [the complaint] status prior to the completion of an investigation and the release of a [report],” the spokesperson said.
Email: ‘I am most concerned about the scheduling’
Mission neurology is divided into two services: one for the ICU and consults, and one for non-ICU patients.
Patients who have suffered life-threatening neurological emergencies are treated in the intensive care unit by neurologists with the help of interventional radiology, critical care doctors and neurosurgeons.
The neurologists admit patients directly to a 12-bed ICU and respond in person to the emergency department for strokes, providing coverage 24 hours a day, seven days a week.
 One of the departing neurologists said it was difficult having to run to the emergency department to treat stroke patients multiple times a day while trying to focus on their other patients.
One of the departing neurologists said it was difficult having to run to the emergency department to treat stroke patients multiple times a day while trying to focus on their other patients.
Responding to emergencies alone could have been a full-time job, the neurologist said, adding the hospital planned to hire someone to do that work, “but that just didn’t happen in time, and it became clear that there was no light at the end of the tunnel over the next year or two.”
Providing telestroke services to regional hospitals also became more difficult, as four such facilities were added to their workload in the past three years, said one of the neurologists.
“Our telestroke volumes have doubled since … 2021 as the result of the additional sites we added,” the neurologist said, adding their jobs also involved “answering phone calls from doctors in hospitals across Western NC for both transfer requests and neurology advice for patients who don’t necessarily need to be transferred.”
The neurologists said they had long been flagging issues, especially in 2023 and early 2024, as patient volume increased and staff changes became inevitable. Two said they tried to work fewer hours two years ago but decided against it, fearing their colleagues wouldn’t have enough support.
According to an email obtained by The Watchdog, one departing neurologist raised concerns at the end of 2023 to three people in HCA management regarding scheduling.
“I am most concerned about the upcoming scheduling, which includes 7 or more days per month of one doctor covering the entire neurology service,” the neurologist wrote. “We have consistently discussed and agreed that to provide adequate care we ideally would be staffed with 3 physicians every day: One for the ICU, one for the floor patients and one for the telestrokes and new consults. … We have been making do with 2 physicians because of our inability to successfully recruit.
“We have been reluctant to consider locums tenens in the past, largely because of concerns of what it would do to our quality, though of late we have all agreed that we must use locums as a stop gap. For unclear reasons, we still don’t have locums on the schedule at this point.
“All of us are working more than our contracts, which is because of our dedication to this group and one another.”
The neurologist then asked a number of questions:
- “What is being done — other than [two neurologists] breaking their backs to provide heroic coverage — to correct the schedule? What is the situation with Locums?
- Why can’t we recruit? Where are the jobs posted? What exactly are the efforts being made? By whom and where and when? Is this crisis in our department being given the priority for the emergency that it is in the administration?
- Is our offer for the position competitive enough for the work that we’re doing?
- What is fair compensation for the additional shifts we are all doing? What monetary incentives to us can the administration offer for each shift that we work over our contracted shifts? It should be at least as much as a locums would be paid.”
The email prompted several meetings between the doctors and Mission administrators, and the hospital did make some changes: It brought on locum tenens and moved to hire a third-party company to provide remote neurologists for night shifts. But the doctors never saw better contracts with more competitive pay, a neurologist said.
Those contracts were “still a work in progress after nine months of meetings,” a departing neurologist said.
‘A violent reaction of nausea and fury’
There was optimism and pride in the neurology group in previous years, all of the neurologists said, even in 2023 as potential staffing deficits loomed.
“The neurology group was really one of a kind in this country, and every single neurologist was an outstanding doctor,” one said. “We had a special chemistry working with each other and we were highly regarded by the nurses and other doctors in the hospital. It is a shame that we ended 2023 with seven staff neurologists and will be ending 2024 with two.”
“The word ‘crisis’ has been used to describe our group situation since January,” another neurologist said. “My group has used that language.”
They believed the hospital would recruit more doctors, the neurologist said. There was even a hope in 2023 that the staff would grow to eight positions.
Another neurologist said they continued working about two years more than they thought they could under the conditions, but “the never-ending acceleration of stroke volume and the aging population, leading to a higher inpatient census of neurologically ill patients at any given time,” ultimately proved too much.
“The hospital has had neurologist job postings to increase the staff numbers for several years now, but numerous promising candidates have turned down our offers, usually citing our night shift work and the abnormally busy inpatient service (for a neurology team),” the neurologist said.
One of the neurologists said HCA didn’t value its staff and showed little desire to retain them.
“HCA considered everyone replaceable, but there’s no economics representing the institutional knowledge that left with them,” the physician said. “I think there is intentional, malignant negligence in getting processes implemented, people hired, contracts offered. HCA offers the usual excuses of any inefficient bureaucracy and claims it’s all national and systemic problems not unique to them.”
Another said they found HCA’s emphasis on profits soon after it purchased Mission to be sickening.
“The speed with which the staffing and resources at Mission were gutted after the acquisition was breathtaking and left little room for doubt about HCA’s priorities,” one departing neurologist said. “I remember sitting through the mandatory corporate training video after the merger and watching their CEO, Sam Hazen, tell us about our obligation to ‘our patients and our shareholders.’ As soon as he mentioned ‘shareholders,’ I had a violent reaction of nausea and fury.”
Asheville Watchdog is a nonprofit news team producing stories that matter to Asheville and Buncombe County. Andrew R. Jones is a Watchdog investigative reporter. Email arjones@avlwatchdog.org. The Watchdog’s reporting is made possible by donations from the community. To show your support for this vital public service go to avlwatchdog.org/support-our-publication/.




The entire deal was compromised by greed, the overseer’s impartiality was questions in the beginning-they sold out the entire western nc community for profit! Now you get terrible service at a dirty and understaffed facility where folks die daily from things that used to be minor or curable and HCA reaps huge profits. The entire deal and players should be investigated and heads should roll-it was crooked from the start but MONEY makes many look the other way?????
The Mission Neuroscience program was once a model for hospitals across the country. The large team of healthcare professionals provided the best stroke care arguably in the entire southeast, expert and compassionate care that I witnessed firsthand when my father had a stroke and was admitted to the stroke team. The physicians and nurses were phenomenal. The remaining few highly skilled healthcare providers can only work so hard and they too will burn out. The community will be left with locum tenens generalist care for a complex disease. This loss is irrecoverable and will lead to worse outcomes and deaths. God forbid I have a stroke one day but if I do, I will be heading to Greenville for a true comprehensive stroke center.