By Christian Green, originally published by Carolina Public Press. Carolina Public Press is an independent, in-depth and investigative nonprofit news service for North Carolina.
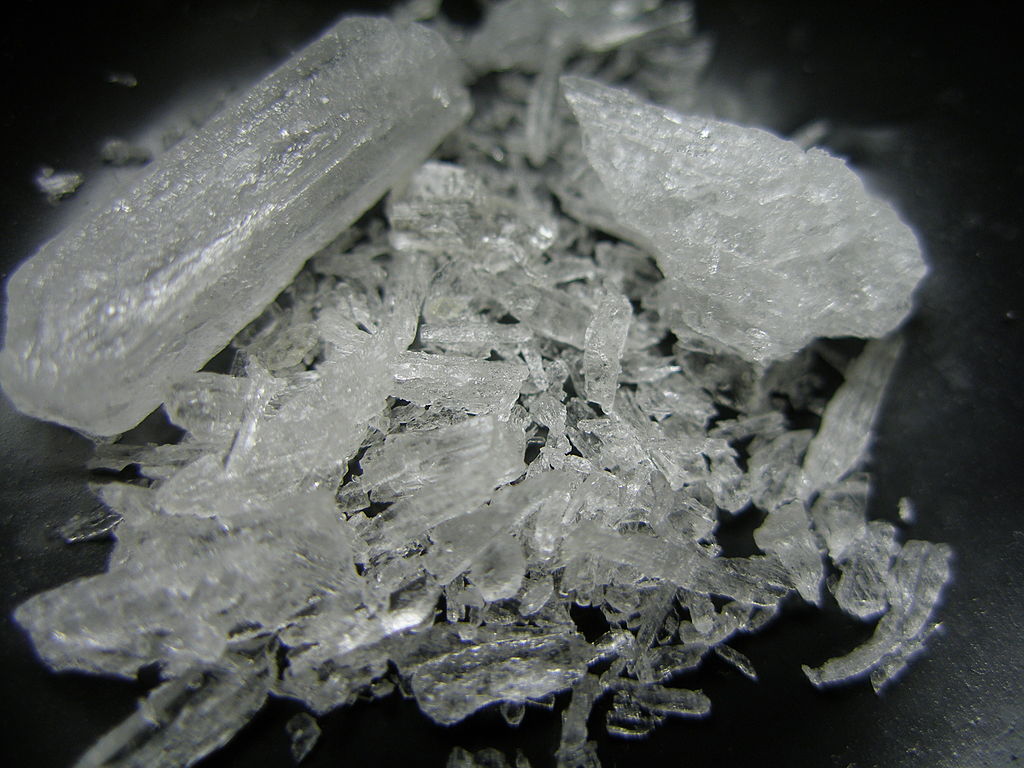
While the opioid crisis gripped many rural areas of the state, the proliferation of methamphetamine challenged communities in Western North Carolina.
“The biggest thing out here in Graham County is meth,” Graham County Health Director Beth Booth said.
“Unlike opioids, with meth, there’s nowhere to point the blame, and no one picking up the staff to fight it,” Booth said.
“There might not be as many deaths directly associated with it, but meth is readily available, it’s really cheap, it ruins lives, and there really is no good treatment.”
Insufficient data
The impact of meth on a specific community is difficult to assess from data, in part because one key data point used to illustrate the severity of a substance is overdose deaths.
While the high rate of opioid deaths indicated the seriousness of the opioid epidemic, the outcomes of meth use were more difficult to decipher because it is less likely to result in a direct overdose death.
In 2018, the state medical examiner told Carolina Public Press 160 people had died during the previous year as a result of methamphetamine-related overdoses. That was less than 10% of the 1,974 opioid-related deaths reported by the state medical examiner in the same year.
But the death rate is only one factor in understanding the effect of meth use on communities.
“I would certainly not want to give the impression that, just because deaths are lower, methamphetamine is somehow less devastating to communities and individuals,” said William T. Stetzer, acting U.S. attorney for the Western District of North Carolina.
“Methamphetamine might not have the same number of overdose deaths, but I think the misery index it brings is still very high as far as communities, tribes and families who are suffering.”
Stetzer, who oversees the prosecution of criminal cases against drug trafficking organizations, described a “significant” increase in the amount of methamphetamine arriving in North Carolina from cartels in Mexico via a supply line that runs through Atlanta to Charlotte, before continuing to Tennessee and then north.
In 2012, U.S. Customs and Border Protection listed that it seized about 18,000 pounds of methamphetamine crossing into the country. By 2018, that number had increased to 85,000 pounds, and in 2020 that number skyrocketed to 177,000 pounds of methamphetamine and crystal meth.
Local producers of meth within communities still exist, Stetzer said, but the influx of high-purity crystal meth had caused prices to decrease by more than half.
“More drugs come in, larger quantities are distributed to local dealers who, in turn, sell even more crystal meth into our communities,” Stetzer said.
Part of polysubstance use
Across the state, 75% of drug-related deaths were caused by multiple drugs taken by a single user, or polysubstance use, according to a recent report by NC Health News.
Polysubstance use compounds the challenge of determining meth’s impact in Western North Carolina.
Though meth is the dominant substance in Graham County, Booth said, it’s not uncommon for people to use multiple substances. Most commonly, they mix meth, a stimulant, with another substance that serves as a depressant, such as opiates.
“Right now, a lot of our participants are mixing meth with heroin or fentanyl,” said Tanasia Boyd, the harm reduction coordinator with Buncombe County Department of Health and Human Services.
In North Carolina, the majority of recent overdose deaths have been among individuals using multiple substances, and nationally the majority of overdose deaths involving stimulants like methamphetamine also involve an opiate.
Over the past two decades, Rebecca Smith, social work division director with the Buncombe County DHHS, has seen different drugs come into and fade out of popularity. Today, though, she said it seems as if illicit substances are more available than ever before. Boyd agreed.
In her experience, Boyd said, not a lot of people of color were using meth. “Now I’m starting to see more and more people,” she said. “It’s everybody. Everybody using everything.”
Treatment challenges
Even for those who are using only meth, receiving care or resources can be more difficult than for those using opiates, Boyd said.
In one situation that Boyd encountered, a woman was using meth and wanted to seek treatment, but she had not yet been using it long enough to qualify for any detox protocols.
“She ended up having to wait a couple of weeks before finally getting in and getting treatment,” she said.
“She’s doing great now, which is good. But if she had had opiates in her system, it would have been automatic. She would have gotten in that day.”
Even when those using meth are able to seek treatment, they face a difficult road because, unlike many other substances including opiates, no approved medication to treat a meth overdose or to alleviate withdrawal symptoms exists currently.
“That’s the biggest difference when treating addiction for meth and for opiates — there are no treatment options for methamphetamine.” said Michael Nader, a professor of physiology and pharmacology at Wake Forest University School of Medicine who specializes in stimulants.
Nader’s colleague Thomas Martin, professor of anesthesiology at Wake Forest who studies pain and opioid abuse, said that when it comes to treating opiate addiction, three approved medications offer options.
Naloxone, also known by its brand name Narcan, is a fast-acting medication that blocks the effects of opioids. It is often used in emergencies to save someone experiencing an opioid overdose.
The other two medications, methadone and buprenorphine, are long-term treatments used to counter addiction to opioids. They are able to prevent or lessen withdrawal symptoms while also decreasing the body’s response to opioids so that an individual is less likely to abuse them in the future.
These drugs are used in combination with other treatments such as therapy and counseling in a process known as “medication-assisted treatment” to aid those who are addicted to opiates.
“It’s honestly generally a lot easier to wean someone off of opioids than it is to get them off meth,” said Booth of Graham County.
“There is no substance-use treatment for meth, so they just have to quit on their own, and that’s really hard. So, it’s kind of counterintuitive, but opioid addiction honestly seems probably like it would be the easier one to tackle.”
Joel Chisholm, an addiction psychiatrist and the behavioral health medical director of the Cherokee Indian Health Authority in Swain County, said he saw a similar dynamic in his clinics.
“We see a lot more people who use opiates engage with treatment because we can provide them medication,” Chisholm said. “The carrots are just a lot bigger for them to engage with treatment versus someone using meth; we still provide them therapy and recovery classes, but it’s a lot tougher.
Ongoing research seeks to create medication that can serve a similar purpose for people who use stimulants, such as cocaine or methamphetamine, Nader said.
Creating treatment drugs in the current climate may be more difficult than in the past, Nader said. Methadone, which was approved for use in treating opioid addiction in the 1960s, would likely not be approved today because it has some potential for abuse, he said.
“The way the FDA has approached potential treatments for stimulant abuse,” Martin said, “… they want something that makes people abstinent but also has pretty much zero abuse liability and of itself. Methadone certainly doesn’t meet that criteria for opioid treatment, so it’s true. There’s a chance it wouldn’t have been approved today.”
Nader said he hopes the U.S. Food and Drug Administration will set out specific guidelines for what it would like to see in a methamphetamine treatment, possibly a drug like methadone, which still has some similar effects, but to a much lesser degree so that it would have less chance to be abused.
In the meantime, while no medication exists for treatment of meth and opioid use continues to receive higher prioritization in many clinics when beds are scarce, it can be difficult for meth users to find help.
“If we have someone coming … off meth (who) wants to get in for treatment and beds are limited, there’s a chance they are actually not going to take them in,” said Samantha Brawley, a peer-support specialist with the Asheville-based Sunrise Community for Recovery and Wellness and a medication-assisted treatment user.
“When that happens, we suggest that they sleep, eat and rest. But sometimes they don’t have a place to sleep, eat or rest, so it becomes a battle. It’s always a battle to try to get somebody in the right place at the right time.”





Before you comment
The comments section is here to provide a platform for civil dialogue on the issues we face together as a local community. Xpress is committed to offering this platform for all voices, but when the tone of the discussion gets nasty or strays off topic, we believe many people choose not to participate. Xpress editors are determined to moderate comments to ensure a constructive interchange is maintained. All comments judged not to be in keeping with the spirit of civil discourse will be removed and repeat violators will be banned. See here for our terms of service. Thank you for being part of this effort to promote respectful discussion.