By Liora Engel-Smith and Rose Hoban, North Carolina Health News
On Oct.7, the Greensboro-based Cone Health system had 57 COVID-19 patients across their small network of hospitals. A month later that number had almost doubled. A month after that, it was up to a total of 167.
And the numbers keep climbing.
“We’re doing this to ourselves,” Bruce Swords, the system’s chief medical executive, told his colleagues.
According to Doug Allred, the system spokesperson, medical leaders at Cone are frustrated, and they’re worried about having enough staff to handle what appears to be a continuing surge of patients.
“In the spring, we shut down everything so we had plenty of staff,” he said. Now, “we’ve got the space and we’ve got the PPE, but you’ve got to be wondering about your staff.”
That’s why this week, Cone launched a targeted public relations campaign urging people in their catchment area of Guilford, Alamance, Rockingham, Randolph and part of Forsyth counties to take a pledge to #MaskUp.
“Wearing a mask is an act of generosity and caring to protect not only ourselves but also other people,” said system head Terry Akin in a press release.
People at other health systems around the state, at hospitals large and small, are expressing similar concerns that people need to do more to arrest the spread of COVID-19. They’re warily eyeing the swelling case numbers, knowing that increased COVID diagnoses eventually turn into increased hospital admissions.
So, they’re pulling out their contingency plans and getting ready.
“We’re concerned, we’re very concerned,” said West Paul, New Hanover Regional Medical Center’s chief clinical officer.
The Wilmington-based health system has enough staff, supplies and beds for now, he said, but as cases and hospitalizations soar across the state, the coming weeks are uncertain.
‘Something has to change’
While cases and hospitalizations are rising across the state, the exact burden of the outbreak differs from region to region. So do the pressure points in each area.
A brief the University of North Carolina’s Sheps Center for Health Services Research and Duke University’s Margolis Center for Health Policy released this week estimates that while the state as a whole may run out of ICU and acute care beds sometime in January, hospitals in the Asheville region, where the pandemic is escalating rapidly, may run out of ICU beds as early as the end of December.
“We project hitting ICU capacity in just less than 5 weeks if current trends persist. If the growth rate were to increase just slightly to 16 percent and hold there, then four weeks would bring us to the edge of ICU capacity,” the authors said.
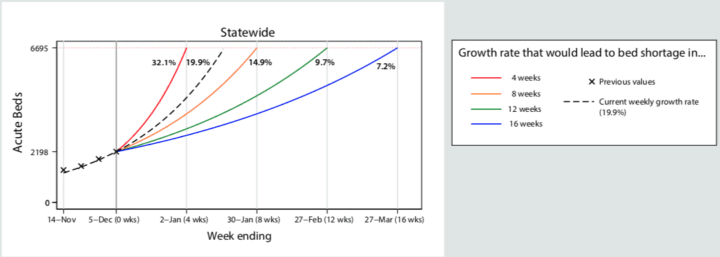

If cases continue to grow at the same rate, the Charlotte region, where hospital capacity is tighter, is projected to run out of acute beds in as little as five weeks, while the Wilmington area has just under 3 months before beds fill to capacity if cases continue to grow at the same rate.
“These numbers are alarming,” said Aaron McKethan, a Duke researcher who co-authored the brief. “On the one hand, we’re a lot better off than many other states and I do think it’s possible that we could avoid dire circumstances that we see in other states.
“On the other hand, what this brief shows is that something has to change.”
That change may not come quickly enough. At a COVID update press conference Tuesday, Health and Human Services Secretary Mandy Cohen said she expected cases to rise as people exposed during the Thanksgiving holiday arrive in emergency departments across the state.
“What we saw last week in our numbers, I think was likely those who went to Thanksgiving already sick,” she said in response to a question about when the state would start seeing the results of holiday gatherings. “What I expect to see this week is people who now are going to be coming back COVID positive because they were with those who were unfortunately sick at Thanksgiving.”
A recent report from the White House Coronavirus Task Force likewise sounded the alarm.
“We are in a very dangerous place due to the current, extremely high COVID baseline and limited hospital capacity,” the report reads. “A further post-Thanksgiving surge will compromise COVID patient care, as well as medical care overall.”
Matching supply with demand
At Vidant Health, the largest hospital system in eastern North Carolina, CEO Michael Waldrum has painted a grim picture of hardships on the horizon. With cases and hospitalizations steadily growing in Vidant’s service area, Waldrum told the Pitt County Board of Commissioners on Monday night, the possibility of care rationing looms large.
“Cases going up will lead to hospitalizations and will lead to deaths about two to six weeks from now,” he said. “We have nothing to stop that reality. Those [patients] who have cases will end up going down those paths.
“The question for us is can we stop that trajectory between now and when there is a solution to the pandemic.”
Waldrum said in an interview this week that suspending elective procedures is not out of the question, but even if the system clears its hospitals, the demand for care may outpace Vidant’s capacity.
Mission Health, a large player in the other end of the state, has made plans to double their ICU bed capacity in two days if the COVID hospitalizations continue to climb. As of Wednesday, a total of 90 COVID patients are at Mission hospitals across the region, said Mission Health spokeswoman Nancy Lindell, most of them are at Mission’s Asheville facility.
“Our hospitalized lab-confirmed positive COVID-19 patients have doubled in the past two weeks and we view this increase as a call to action for each and every member of our community,” she wrote.
Erlanger Western Carolina Hospital in Murphy, another mountain region hospital is preparing for a potential surge.
“At this time, Erlanger Western Carolina Hospital is not overwhelmed due to COVID-19, but we are aware that this situation could change at any moment,” said Teresa Bowleg, director of operations and associate chief nursing officer.
Novant, a giant in the Charlotte region, has likewise prepared for a surge by stepping up its number of staffed beds.
“With investments and tireless efforts, we have been able to increase our bed capacity by 60% and have worked to reinforce our supply chain,” spokeswoman Kristen Barnhardt said in an email. “We are carefully monitoring our capacity and, at this time, we have additional patient capacity.”
In some places, it appears, the surge has already begun.
The Statesville-based Iredell Health System reports their COVID caseload has ticked up 45 percent in the past two weeks. That’s even as system leaders describe using a “hospital at home” approach to manage patients who need care but don’t necessarily need admission.
The 18 counties that comprise the Triad Healthcare Preparedness Coalition, which includes Iredell Health, have had the heaviest load of cases over the past month. The area has consistently had about 20 percent of the state’s population, but hospitals in the region have had around 30 percent of the hospital and ICU admissions.
“We are very worried at this time,” wrote Joseph Mazzola, chief medical officer for Iredell Health wrote. Asked to sum up his feelings, he responded, “Overwhelmed with concern.”
Staff shortages a concern
Even as the crisis unfolds on different timelines, the Sheps/Margolis brief points out that the state’s health care workforce shortage can make matters worse, particularly because every region will need its workforce, so sharing staff between regions won’t be feasible.
“We can’t call for help and ship nurses in because everybody is in this phase and the national workforce is tired and stressed,” said Waldrum, Vidant’s leader. “There’s no release valve anymore.”
As the pandemic drags on, retaining staff has become even more important. Staff is not immune to the disease, and they can’t work when they get sick, Waldrum said. The health system is roughly two weeks away from vaccinating health care workers against coronavirus.
“Everybody is talking about the vaccine and it’s great, we need it, and it’s important but it’s not important today … It will have no effect for a while,” he said. “Our house is on fire today.”
North Carolina Health News is an independent, nonpartisan, not-for-profit, statewide news organization dedicated to covering all things health care in North Carolina. Visit NCHN at www.northcarolinahealthnews.org.
This article first appeared on North Carolina Health News and is republished here under a Creative Commons license.




Before you comment
The comments section is here to provide a platform for civil dialogue on the issues we face together as a local community. Xpress is committed to offering this platform for all voices, but when the tone of the discussion gets nasty or strays off topic, we believe many people choose not to participate. Xpress editors are determined to moderate comments to ensure a constructive interchange is maintained. All comments judged not to be in keeping with the spirit of civil discourse will be removed and repeat violators will be banned. See here for our terms of service. Thank you for being part of this effort to promote respectful discussion.