By Neil Cotiaux, originally published by Carolina Public Press. Carolina Public Press is an independent, in-depth and investigative nonprofit news service for North Carolina.
Editor’s note: COVID-19 poses an increased risk for severe illness or death in people over 65 years of age. Carolina Public Press previously identified 20 North Carolina counties that have the highest percentage of their population in the high-risk age range for COVID-19, nearly all of them rural. This is the final installment in a six-part series looking at hospitals and health infrastructure in those counties. This article focuses on a cluster of six mountain counties, including Henderson, Polk, Transylvania, Macon, McDowell and Mitchell.
Four months have now passed since an outbreak of COVID-19 erupted at Cherry Springs Village, a congregate living facility in Hendersonville, in North Carolina’s central mountains.
While the assisted living center’s outbreak is now over, the disease caused by the new coronavirus has more recently affected eight skilled nursing homes in Henderson and Buncombe counties.
As of Aug. 4, according to the N.C. Department of Health and Human Services, the disease had claimed a combined five lives among 197 infected individuals at those facilities, and that represents a decline in such outbreaks in the two counties.
“Our percentage of 65-and-older in Henderson County is 28%,” said Anna Hicks, a geriatrician with WNC Family Medical Center who regularly sees patients at long-term care facilities. “Many of those are in long-term care beds.”
“We have over 35 core licensed care facilities in Henderson County, which include larger group homes, independent living, assisted living and skilled nursing,” said Jimmy Brissie, Henderson County’s emergency services director.
Shared space, the daily arrival of staff from outside and visits from family can help spread COVID-19 in those kinds of close quarters, experts say.
When the first positive cases surfaced at Cherry Springs Village in April, Hicks and Brissie assembled a team of specialists to consult with management on the center’s needs and best practices that could be used to mitigate the outbreak.
“It was more of a proactive measure, that we would be able to deal with anything that came up rather than wait,” Hicks told Carolina Public Press.
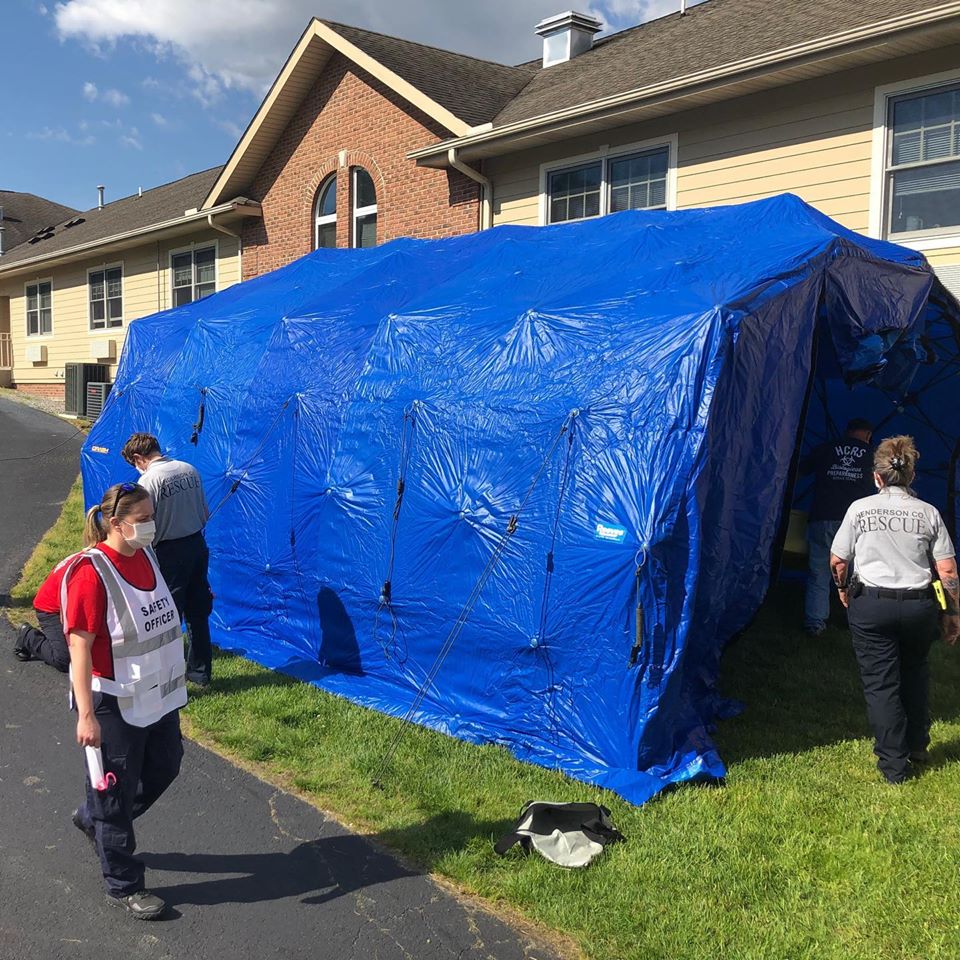
After working with the center’s staff and patients for more than a month, the two took what they learned from their experience and created a formal “strike team” model that could be employed at other congregate living facilities.
The strike team consists of a team leader, medical provider, nurses, emergency medical technicians, logistics and supply chain experts, and others who work alongside the properties’ owners or managers but who do not override their authority.
The group offers advice and direction on creating quarantine space, sanitizing, the donning and doffing of personal protective equipment, the use of skilled nurses who are not ordinarily available at assisted living centers, contact with family members and other practices.
To date, Henderson County’s strike team has visited nearly two dozen facilities before any outbreak with the hope of fully preparing them for a worst-case scenario.
“We picked out some of the larger independent living, assisted living and skilled nursing facilities for site visits and were able to visit 20 of them for assessments,” Brissie said.
Other counties in Western North Carolina have adopted the model for use in their own congregate living settings.
Statewide, through the end of August, up to 70,000 nursing home residents and staff will have undergone voluntary screenings for the coronavirus in an outreach program conducted by pharmacy chain CVS, under contract and in partnership with NCDHHS.
Mission Health cases increase
Across the state, the number of positive COVID-19 cases and related hospitalizations have risen since June and now appear to have leveled off a bit, but the longer-term trend remains unclear.
“At the beginning of July, we were averaging around 20-25 (COVID-19) patients in the hospital, and then more recently we’re up in the low 40 range, 40-45 patients in the hospital on average at a given time,” said William Hathaway, chief medical officer at Mission Hospital, in an Aug. 4 statement.
The Asheville facility serves many patients from across Western North Carolina. Several rural counties have their own Mission-run hospitals, including Macon, Transylvania, Mitchell and McDowell counties. But the sickest patients in these rural mountain counties, including some with COVID-19, often go to Mission in Asheville for care.
“We still have adequate capacity from a room point of view, from an intensive care unit point of view, from a protective equipment point of view and testing supplies to handle this volume right now,” Hathaway said.
The vast majority of in-hospital testing for COVID-19 is completed rapidly, said Sam Hazen, CEO of Mission’s parent company, HCA Healthcare.
“Currently, 90% of COVID-19 lab results are produced in less than 48 hours,” Hazen told a group of financial analysts.
AdventHealth Hendersonville is also seeing an increase in positive cases through testing and admissions, spokesperson Victoria Dunkle said, with the capability of utilizing 26 ICU beds if needed at full-surge level.
Pardee UNC Health, also in Hendersonville, had four COVID-19 patients in the hospital as of Aug. 5, and its rolling seven-day average was 3.4 patients, said spokesperson Amy Holcombe.
In addition to caring for infected patients, the three area hospitals are also engaged in convalescent plasma therapy.
“Antibodies collected from patients who have recovered from COVID-19 appear to be effective in targeting the virus when given to patients hospitalized with the infection,” said Christopher Parsons, medical director of the Pardee Center for Infectious Diseases, in a recent press release.
“Collective results from people receiving the treatment can provide information about the effectiveness of the therapy and whether it can become an approved therapy to treat COVID-19 infection,” the release said.
In-house testing at hospitals
Currently, area hospitals are mostly focusing on in-house testing and not widespread public testing.
“At Mission right now, we are testing patients who come to us in our walk-in clinics or our practices who are actively sick,” Hathaway said. “We are testing anyone who, of course, comes to our emergency department.
Mission facilities are also assessing which patients admitted for surgery may need to be tested for COVID-19 as well, he said.
Pardee’s primary care offices do not currently provide COVID-19 testing but its urgent care facility in Fletcher evaluates and tests patients who exhibit symptoms of the disease, said David Ellis, chief medical officer. The hospital also performs COVID-19 testing for all preoperative patients and symptomatic patients admitted.
AdventHealth provides COVID-19 testing for patients ahead of invasive procedures and for patients sent to them by providers in its care network. Other members of the public who want testing can visit AdventHealth Centra Care in Arden.
Partnership helps St. Luke’s
In rural Polk County, about an hour southeast of Asheville, Columbus-based St. Luke’s Hospital has found that partnering with a regional health care system can reduce frustration among patients who want to know if they are infected with the new coronavirus.
Now in its 90th year, the nonprofit hospital draws patients from an older, rural population that is considered to be at high risk for COVID-19.
“Initially as the country entered the pandemic, St. Luke’s was waiting sometimes two to three weeks to get a lab result back from their vendor to learn if an individual was COVID-19 positive,” said Michelle Fortune, CEO of the 25-bed critical access hospital.
“This created a challenge with burning through PPE, because until it is known that the patient is negative, PPE must be worn to the level of a positive result to ensure safety.
“Partnering with Atrium Health, St. Luke’s was able to get lab results within 24 hours, and this allowed conservation of very difficult-to-resource items like N95 masks.”
St. Luke’s first contracted with Atrium (formerly Carolinas HealthCare System of Charlotte) in 2008 for specified management services, including guidance on productivity and expenses and participation in purchasing contracts.
During the pandemic, Fortune said, hospital staff has had the ability to interact with infection prevention specialists from Atrium and utilize the system’s protocols and guidelines.
St. Luke’s provides a steady stream of elective surgery and the suspension of such services due to COVID-19 this spring had a “dramatic financial impact,” Fortune said.
Over the years, St. Luke’s has benefited from financial support from The Duke Endowment, Polk County Community Foundation, Polk County Economic Development and the St. Luke’s Hospital Foundation.
Other articles in this series
Cherokee, Clay, Graham counties: Slow start to pandemic in SW NC counties but future of hospitals uncertain
Brunswick County: Brunswick medical providers coordinate pandemic efforts in retiree haven
Chatham, Moore counties: Central NC health systems battle outbreaks, but confident of preparations
Ashe, Allegany counties: Provider partnerships crucial to NC rural hospitals in NW mountains
Beaufort, Washington, Carteret, Pamlico, Chowan and Perquimans counties: Hospital’s new owner rocks Plymouth with Texas-sized vision for northeastern NC counties





Before you comment
The comments section is here to provide a platform for civil dialogue on the issues we face together as a local community. Xpress is committed to offering this platform for all voices, but when the tone of the discussion gets nasty or strays off topic, we believe many people choose not to participate. Xpress editors are determined to moderate comments to ensure a constructive interchange is maintained. All comments judged not to be in keeping with the spirit of civil discourse will be removed and repeat violators will be banned. See here for our terms of service. Thank you for being part of this effort to promote respectful discussion.